The science is out there, but you won’t read about it
When my son came to me saying he felt he was trans, my first inclination, being a scientist, was to dive into the research. I wanted to understand, from a medical and scientific perspective, what was going on with my son. I figured the science was settled, there were evidence-based studies that I could reference. I thought that I was capable of understanding what my son was going through, if I could just understand the science. As his dad, I was determined to accomplish this, for him and for our family.
It didn’t take long for me to discover, however, that this was simply not going to be possible. I’m now convinced that trans is not based on science. It’s fundamentalist religious ideology disguised as science. And not only that, because the entire field is being represented as science when it is, in fact, a belief system, information about extremely harmful side effects is being suppressed, and research efforts are completely subverted, because the ultimate goal is to support the ideology at all costs.
What’s most despicable about the whole affair is that the science is out there showing that the risk/benefit balance is way off when it comes to transgender medical interventions, but medical professionals and researchers are not looking at the data. Because they don’t want to know. So, it’s left to parents like me to do the heavy lifting and become the experts. This is wrong.
From my own experience with my son, it’s clear to me that these children DO feel deeply that they have issues with their body. That is not in question. I know my young teen son feels deeply that he is a woman, or at least that’s what he tells me. I also know that there are likely other underpinning reasons why he feels this way other than that he is literally a woman trapped in a male body. And, I think he is aware that he is not actually a woman, a situation which causes inherent cognitive dissonance. But through today’s rigid ideological lens, that is the only possibility offered to him from the gurus online and, similarly, there is only one possible treatment – trans medicine. But, actually, the science says that one size cannot fit all. At a time when cancer care is based on genetically modifying individual DNA, transgender medicine is still in medieval age of one size fits all – Puberty Blockers, Cross Sex Hormones, and Surgery. Trans is the medical version of the Taliban.
This one-size-fits-all approach is a recent phenomenon. Even when transgenderism was mainly an adult medical field and quite rare in its presentation at clinics, studies have shown that, depending on the presentation, differential diagnosis led to different treatment pathways to produce the best possible outcome for the patient to relieve their symptoms. And these different options and paths were explored, over extended time periods, with each case. The results showed that action short of full sex reassignment (in a legal and medical sense) sometimes yielded positive results.
There was, for instance, the case of a physician who observed that, as they reduced the patients’ testosterone levels, their desire to identify as the opposite sex completely went away. Medically, this makes perfect sense. The brain is clearly impacted by hormonal changes in the body and that the brain is an endocrine organ. Would it not make sense then, to understand if there is a chemical basis for these feelings that can be addressed, short of “transition”. In other words, what are the impact of hormones on the brain?
There ARE studies available about the impacts of trans-medicalization (specifically wrong sex hormones) on the brain — and the results are not good at all. However, unfortunately, no one has made the effort to translate these studies into plain English. It’s far easier to say all gender identities are valid and hormones are no big deal, then to read a complex scientific paper.
As a scientific minded parent, I think it’s essential that we take the time to do just that—after all our children’s medical and mental health is at stake. Unfortunately, the results from the studies out there show that the effects of so-called transgender medicine are horrible.
Gender ideologues say that taking estrogen “feminizes” the brain. It does no such thing. What it appears to do is change blood flow, reduce the size of the brain, interfere with executive function, cause dangerously high build-ups of glutamate, and lead to early-onset dementia and high risk of stroke.
The summary of the effect of estrogen is as shown below, with associated long term risk factors linked to morphological changes or serum marker changes. In sum, estrogen introduced in male brain leads to high glutamate levels, reduction of the size of the brain, and increase in the size of ventricles. Long term, these studies are revealing that estrogen in males leads to reduction in grey matter and vastly increases the risk of Alzheimer’s Disease and psychopathology. These are serious brain changes with extremely serious long term side effects.
What’s worse, this research has been available to the medical community for decades with the first transgender brain morphology study published in 2006 by HeH Pol et al, and replicated by Zubiaurre-Elorza et al in 2014, Sieger et al, Mueller et al, and several others in subsequent years. In 2020, Gomez et al replicated the morphology studies (hippocampal volume reduction, ventricular volume expansion) in mice models and also showed high glutamate levels in the brain on Estradiol treated male mice.
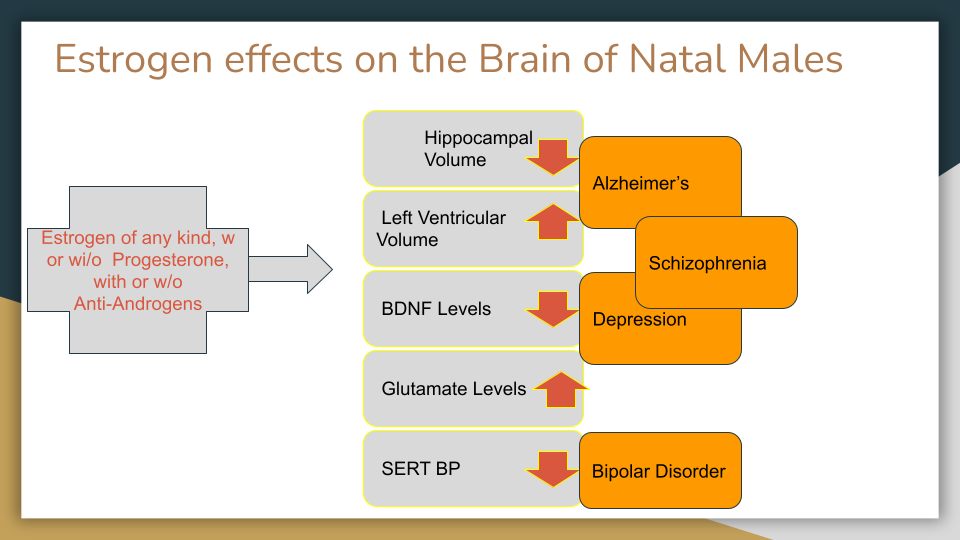
Mueller et al, observed in their structural MRI study of persons on wrong sex hormones, that “Ventricular enlargement has not only been associated with grey matter reduction due to aging , but has also been identified as a putative marker for progression of Alzheimer’s Disease or a risk factor for psychopathology. Hulshof Pol observed a final 3rd ventricle size in transgender women on hormonal therapy that was larger after treatment than the ventricle size observed in both natal men and women. Although the mechanisms and clinical implications of such effects are unknown, they deserve further study given reports of physiological risk with hormonal treatment and prevalence of psychopathology in transgender persons”.
Kraguljac et al, observed in their study on the Pathophysiological Mechanisms of Schizophrenia “glutamatergic hyperactivity is hypothesized to be a key pathological feature in schizophrenia. Glutamate neurotransmitter flux, neuronal firing rate, and the blood oxygen level dependent (BOLD) response are tightly coupled, and glutamate plays a role in long-range functional connections. In preclinical studies, excess glutamate has been shown to be associated with disorganized neuronal activity and may result in increased synapse turnover as well as axonal or glial injury. We also conducted studies to examine the impact of glutamate (excess) on brain structures. In unmedicated chronic schizophrenia patients, we found that higher hippocampal glutamate was associated with lower hippocampal volumes, suggesting that glutamate related excitotoxicity (neurotransmitter excess related increased synapse turnover) might affect brain structure.
These are all alarming effects on the brain that should be a reason for a pause on experimental therapies with estrogen on males. From a scientific basis, we should not be giving males estrogen. It’s as simple as that. It’s imperative that we prioritize other ways to address gender distress, because introducing wrong sex hormones is not safe.
Medically, exogenous estrogen isn’t safe for males (or for females for long term use). However, it’s not safe or effective for mental health either, it turns out. Apart from these cause-effect studies, several long range studies and transgender mental health surveys show significant mental health challenges in transgender identified persons. Pachankis et al, showed that, in a longitudinal study of over a decade of persons on hormonal or surgical “transition” treatment on data from the entire population with no drop-outs, mental health did not improve with such treatments. So, not only are the risks high, and the brain impacts severe, there is no evidence that they even help the patient with their original issue.
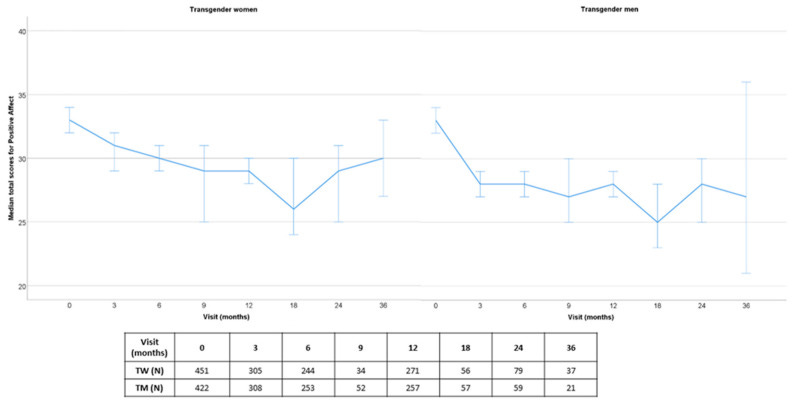
In 2020, ENIGI published a longitudinal study that showed a similar result in a deliberately tracked group over three years.
A 2021 study presented at AIAC conference showed a substantially higher cognitive decline in transgender identified persons.
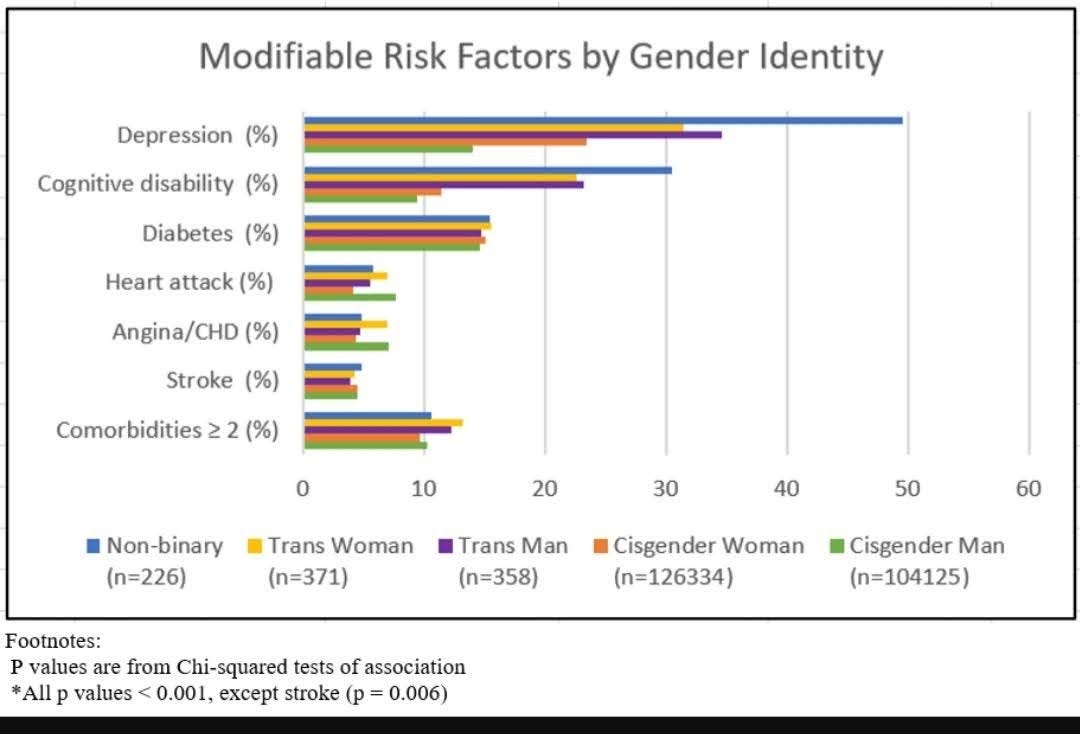
The higher cognitive decline (in the 12 months leading to the survey date) was observed at a statistically younger age. As indicated by a study author in a tweet, the study could not determine whether the persons surveyed were ever on hormones, while agreeing this was an important factor to consider.
In a 2019 survey of 25,233 transgender identified patients compared to Cisgender patients in a hospital discharge setting, B Hanna et al observed the following alarming statistics:
“The prevalence of mental disorder diagnoses was higher in transgender hospital encounters (77% vs. 37.8%, P < .001). The prevalence of each examined mental disorder diagnosis was significantly higher in transgender hospital encounters. A multivariable analysis demonstrated significantly higher odds of all mental disorder diagnoses (odds ratio [OR] = 7.94; confidence interval [CI], 7.63–8.26; P < .001). Transgender encounters with a mental disorder diagnosis had a higher prevalence of chronic medical co-morbid diagnoses as compared with transgender encounters without mental disorder diagnoses.”
Additionally, in a 2011 longitudinal study by Dhejne et al, over a 13 year period , with no loss to follow up, sexually reassigned males (on hormones and surgery) had psychiatric hospitalization at 2.5X the rate of control males and suicidality at 2X the control. In a study published this month ‘Mortality trends over five decades in adult transgender people receiving hormone treatment: a report from the Amsterdam cohort of gender dysphoria’ the author’s looked at a total follow-up time of 40,232 person-years for Males on wrong sex hormones. During follow-up, 10·8% transgender women died, which was higher than expected compared with general population men (Standardized Mortality Ratio -SMR 1·8, 95% CI 1·6–2·0) and general population women (SMR 2·8, 2·5–3·1). Cause-specific mortality in the hormone treated cohort was high for suicide, consistent with the Dhejne study . Importantly, No decreasing trend in mortality risk was observed over the five decades studied.
If you glean nothing else from these studies, it is at least clear that the balance of risk versus benefit for these serious medical interventions merits discussion and consideration.
Unfortunately, however, this is not the case. Debate has been stifled; these studies buried. Lacking public debate, it’s been left to parents like me, capable of reading dense scientific papers and studies, to try to interpret the details and make informed decisions. At the most charitable interpretation for this willful disregard of the science, the medical community simply assumes that these medical interventions must be safe, or they wouldn’t be trumpeted in the New York Times and other trusted publications. More likely, medical professionals continue to look the other way to continue to financially benefit from confused kids and young adults, and to avoid future legal liability by remaining in ignorance.
In a recent paper on the research gaps in medicalization of gender confused persons, over a hundred papers were surveyed, however not a single brain cause effect research was included in the study. The study authors simply concluded that hormonal treatments result in a transference of risk to the desired sex. Decades of neuro-imaging studies indicate that if these studies are included there is overwhelming evidence to show that the brain effects such as ventricular expansion are a significant risk factor for cognitive decline.
Even for women, the effects and risks of exogenous estrogen are serious. These effects of exogenous estrogen on ventricular volume expansion has been studied in a cohort of Natal women in the KEEPs study, by Mayo Clinic Researchers. Due to these risk factors and breast cancer risks that have been extensively studied in women due to exogenous estrogen combined with any form of progesterone (including Micronized progesterone), the non profit USPSTF has recommended against Estrogen and Progesterone HRT for even limited periods of time, for post menopausal women. USPSTF stated in their recommendation that the risks outweigh any benefits. But yet, this is administered readily, for a lifetime’s use, to boys and young men?
The open disregard of scientific evidence of harmful effect of exogenous hormones on the brain, and other organs shows that at least in the US, Transgender medicine is more akin to a fundamentalist religious movement, than to a well debated, questioning, scientific research process.
Sources:
- Christel JM de Blok, MD
- Chantal M Wiepjes, PhD
- Daan M van Velzen, MD
- Annemieke S Staphorsius, MSc
- Nienke M Nota, PhD
- Louis JG Gooren, PhD
- Baudewijntje PC Kreukels, PhD
- Prof Martin den Heijer, PhD
- Show less
Published:September 02, 2021DOI:https://doi.org/10.1016/S2213-8587(21)00185-6
Flatt, Jason D et al. “Subjective cognitive decline higher among sexual and gender minorities in the United States, 2015-2018.” Alzheimer’s & dementia (New York, N. Y.) vol. 7,1 e12197. 28 Jul. 2021, doi:10.1002/trc2.12197 https://www.alz.org/aaic/releases_2021/transgender-adults-cognition.asp
Fuss J, Hellweg R, Van Caenegem E, Briken P, Stalla GK, T’Sjoen G, Auer MK. Cross-sex hormone treatment in male-to-female transsexual persons reduces serum brain-derived neurotrophic factor (BDNF). Eur Neuropsychopharmacol. 2015 Jan;25(1):95-9. doi: 10.1016/j.euroneuro.2014.11.019. Epub 2014 Dec 4. PMID: 25498415. https://pubmed.ncbi.nlm.nih.gov/25498415/
Gómez Á, Cerdán S, Pérez-Laso C, Ortega E, Pásaro E, Fernández R, Gómez-Gil E, Mora M, Marcos A, Del Cerro MCR, Guillamon A. Effects of adult male rat feminization treatments on brain morphology and metabolomic profile. Hormones and Behavior. 2020 Sep;125:104839. doi: 10.1016/j.yhbeh.2020.104839. Epub 2020 Aug 22. PMID: 32800765. https://pubmed.ncbi.nlm.nih.gov/32800765/
Hanna B, Desai R, Parekh T, et al. Psychiatric disorders in the U.S. transgender population. Annals of Epidemiology. 2019 Nov;39:1-7.e1. DOI: 10.1016/j.annepidem.2019.09.009. PMID: 31679894. https://europepmc.org/article/med/31679894
Hulshoff Pol, H. E., Cohen-Kettenis, P. T., Van Haren, N. E. M., Peper, J. S., Brans, R. G. H., Cahn, W., Schnack, H. G., Gooren, L. J. G., & Kahn, R. S. (2006). Changing your sex changes your brain: Influences of testosterone and estrogen on adult human brain structure. European Journal of Endocrinology, Supplement, 155(1). https://doi.org/10.1530/eje.1.02248
Ihara K, Yoshida H, Jones PB, Hashizume M, Suzuki Y, Ishijima H, Kim HK, Suzuki T, Hachisu M. Serum BDNF levels before and after the development of mood disorders: a case-control study in a population cohort. Transl Psychiatry. 2016 Apr 12;6(4):e782. doi: 10.1038/tp.2016.47. PMID: 27070410; PMCID: PMC4872405. https://pubmed.ncbi.nlm.nih.gov/27070410/
Kantarci K, Tosakulwong N, Lesnick TG, Zuk SM, Lowe VJ, Fields JA, Gunter JL, Senjem ML, Settell ML, Gleason CE, Shuster LT, Bailey KR, Dowling NM, Asthana S, Jack CR Jr, Rocca WA, Miller VM. Brain structure and cognition 3 years after the end of an early menopausal hormone therapy trial. Neurology. 2018 Apr 17;90(16):e1404-e1412. doi: 10.1212/WNL.0000000000005325. Epub 2018 Mar 21. PMID: 29661902; PMCID: PMC5902783. https://pubmed.ncbi.nlm.nih.gov/29661902/
Kraguljac NV, Lahti AC. Neuroimaging as a Window Into the Pathophysiological Mechanisms of Schizophrenia. Front Psychiatry. 2021 Mar 11;12:613764. doi: 10.3389/fpsyt.2021.613764. PMID: 33776813; PMCID: PMC7991588. https://pubmed.ncbi.nlm.nih.gov/33776813/
Kranz GS, Wadsak W, Kaufmann U, Savli M, Baldinger P, Gryglewski G, Haeusler D, Spies M, Mitterhauser M, Kasper S, Lanzenberger R. High-Dose Testosterone Treatment Increases Serotonin Transporter Binding in Transgender People. Biol Psychiatry. 2015 Oct 15;78(8):525-33. doi: 10.1016/j.biopsych.2014.09.010. Epub 2014 Sep 23. PMID: 25497691; PMCID: PMC4585531. https://pubmed.ncbi.nlm.nih.gov/25497691/
THE LANCET DIABETES & ENDOCRINOLOGY: Mortality risk in transgender people twice as high as cisgender people, data spanning five decades suggests https://www.thelancet.com/journals/landia/article/PIIS2213-8587(21)00185-6/fulltext
Lawrence, Anne A. Men Trapped in Men’s Bodies: Narratives of Autogynephilic Transsexualism. New York, NY: Springer, 2013. Internet resource, p. 150. https://www.springer.com/gp/book/9781461451815
Matthys, Imke et al. “Positive and Negative Affect Changes during Gender-Affirming Hormonal Treatment: Results from the European Network for the Investigation of Gender Incongruence (ENIGI).” Journal of clinical medicine vol. 10,2 296. 14 Jan. 2021, doi:10.3390/jcm10020296 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7829763/
Mueller SC, Landré L, Wierckx K, T’Sjoen G. A Structural Magnetic Resonance Imaging Study in Transgender Persons on Cross-Sex Hormone Therapy. Neuroendocrinology. 2017;105(2):123-130. doi: 10.1159/000448787. Epub 2016 Aug 5. PMID: 27490457. https://pubmed.ncbi.nlm.nih.gov/27490457/
Mueller SC. Mental Health Treatment Utilization in Transgender Persons: What We Know and What We Don’t Know. Am J Psychiatry. 2020 Aug 1;177(8):657-659. doi: 10.1176/appi.ajp.2019.19111151. PMID: 32741290. https://ajp.psychiatryonline.org/doi/epub/10.1176/appi.ajp.2019.19111151
Mueller SC. Mental Health Treatment Utilization in Transgender Persons: What We Know and What We Don’t Know. Correction. https://ajp.psychiatryonline.org/doi/10.1176/appi.ajp.2020.1778correction
Safer JD. Research gaps in medical treatment of transgender/nonbinary people. J Clin Invest. 2021 Feb 15;131(4):e142029. doi: 10.1172/JCI142029. PMID: 33586675; PMCID: PMC7880308. https://pubmed.ncbi.nlm.nih.gov/33586675/
Seiger R, Hahn A, Hummer A, Kranz GS, Ganger S, Woletz M, Kraus C, Sladky R, Kautzky A, Kasper S, Windischberger C, Lanzenberger R. Subcortical gray matter changes in transgender subjects after long-term cross-sex hormone administration. Psychoneuroendocrinology. 2016 Dec;74:371-379. doi: 10.1016/j.psyneuen.2016.09.028. Epub 2016 Oct 5. PMID: 27744092. https://pubmed.ncbi.nlm.nih.gov/27744092/
Stute P, Wildt L, Neulen J. The impact of micronized progesterone on breast cancer risk: a systematic review. Climacteric. 2018 Apr;21(2):111-122. doi: 10.1080/13697137.2017.1421925. Epub 2018 Jan 31. PMID: 29384406. https://pubmed.ncbi.nlm.nih.gov/29384406/
U. S. Preventive Services Task Force Recommends Against Hormone Therapy for Preventing Chronic Conditions in Postmenopausal Women. For women who have gone through menopause, benefits do not outweigh harms of using hormone therapy to prevent chronic conditions. https://www.uspreventiveservicestaskforce.org/uspstf/sites/default/files/file/supporting_documents/hormone-therapy-finalrs-bulletin.pdf
Zubiaurre-Elorza L, Junque C, Gómez-Gil E, Guillamon A. Effects of cross-sex hormone treatment on cortical thickness in transsexual individuals. J Sex Med. 2014 May;11(5):1248-61. doi: 10.1111/jsm.12491. Epub 2014 Mar 11. PMID: 24617977. https://pubmed.ncbi.nlm.nih.gov/24617977/
Note: The 100 reference article by the head or USPATH does not refer to brain morphology research at all
Originally published at https://pitt.substack.com/p/rise-of-the-trans-medical-taliban reproduced by kind permission.

