aka Trans Medical Taliban Part II
The ugly truth: Trans medicine is not about fixing a natural condition of being born in the wrong body, as activists would have you believe. And it is certainly not a journey to become one’s true self, which should not require any drugs or surgeries. It doesn’t actually turn a man into a woman, or vice versa, either. The goals are unclear, unarticulated, and undefinable when it comes down to it. What it seems to be, instead, is an uncontrolled chemical experiment on the human brain, sometimes with debilitating cosmetic surgery on the body in tandem.
In this societal experiment, gender dysphoria, which develops in the brain, potentially from rumination on gender roles and dysphoria itself, is reinforced by wrong-sex chemical interventions in the form of hormones. In the manner of a self-fulfilling prophesy, these hormones change and damage neural pathways that affect one’s sense of self—the same pathways that play into eating disorders. They destroy and disrupt brain connections, damage astrocytes (the “glue cells” of the nervous system), and reduce brain mass and volume, with all the resultant impacts on brain function that one might imagine. And, contrary to these same activists’ claims, there is no silver bullet that protects the brain from the devastation that hormones inflict. For males, progesterone does not mitigate the damage that high levels of estrogen have on the male brain.
This article summarizes my continuing research on the topic since Rise of the Trans Medical Taliban, an article with an inflammatory title, but one that I stand behind. Gender medicine is harming people, including kids, teens, and young adults, in the name of a radical, fundamentalist ideology. It has no basis in cause-and-effect scientific or evidence-based medicine, and the horrifying long-term results demonstrate this. Again, parents are filling in the information void, while doctors continue to hide their heads in the sand. And again, I (and other parents I know) have found that the research out there does not support the safety or efficacy of gender medicine. Experimenting on the minds of our children and young people through wrong sex hormones, and experimenting on their bodies through cosmetic surgeries meant to craft facsimiles of the desired opposite sex, can only lead to tragedy and human suffering. And, it already is.
Gender Dysphoria and Changes in the Resting State Networks
It is becoming increasingly evident that Gender Dysphoria is not a case of having an opposite sex gendered brain in your body—a belief with no basis in science or logic. Instead, evidence points to connectivity within the Resting State Networks of the brain to explain why some feel that they are the opposite of their actual sex. Namely, research indicates that, with gender dysphoria, as with anorexia nervosa and other body dysmorphia disorders, there are visible connectivity changes within the Default Mode (DMN) and Salient (SN) Networks, which are believed to be the neurological basis for the sense of self.
In their study of brain morphology and on the possible neurobiological underpinnings of Gender Dysphoria, Savic et al conducted a study of brain differences in individuals that expressed gender dysphoria. What they found is that the brain morphology of gender dysphoric individuals was indistinguishable from their natal sex, once adjusted for homosexuality (interestingly, there were differences noted between homosexual and heterosexual individuals). There were changes, however, in gender dysphoric individuals, not in the brains themselves, but in the neuroplastic connectivity networks responsible for “mediating self–body perception”— showing decreased communication in individuals with dysphoria. Because of these connectivity changes, they noted that they were unable to determine that gender dysphoria is innate, or if instead, it is the result of long-term rumination.
Similar findings have been made in studies of anorexia patients. Similar to the gender dysphoria studies, researchers found that there was weakened functional activity in the DMN, and microstructural abnormalities in fronto-occipital brain structure in patients with anorexia, a disorder that has, at its root, a similar disconnect between the image of self and the body, in this case, body weight and size, rather than gender. These disorders appear to be more similar than activists would have us believe, and both involve a disconnect between biological reality and self that is observable within the brain.
In the case of both gender dysphoria and anorexia, the cause and effect is unclear— did a mental disconnect in the subjects, between “their own body image and perception of self”, potentially due to rumination and social influences (known causal factors for both ailments), subsequently lead “to a weakening of the structural and functional connections in these networks”, or did weakened connections and decreased connectivity create the chasm or dysphoria in the person’s sense of self? More study is needed to address the root causes. However, it is clear that disrupted neural pathways can disrupt the sense of self and lead to a variety of distressing conditions.
However much activists would like to believe that these afflictions are different, the brain says otherwise. The commonalities between Anorexia and Gender Dysphoria patients are so evident, that it is striking that this is continually overlooked by researchers. Equally striking, however, are the very different ways that these two disorders are treated, because the common root cause or symptom is being overlooked. Anorexia is treated through psychological care, whereas gender dysphoria is currently treated through affirmation and medicalization to support the disordered thinking. These divergent treatment protocols are baffling. Physicians and psychologists treating eating disorders never affirm the observably false idea, caused by the disruption in accurate body perception, that the patient is overweight, and it is known that eating disorders can be resolved by following this approach, in combination with supportive medical care. With gender dysphoria, however, the school of thought is to agree with the patient’s observably false perception of self and to undertake medical and psychological treatments that further enhance the dysphoria.
Now, when wrong sex hormones are introduced into these individuals with mental dissociation, neural networks are further disrupted by this chemical intervention. As the study by Clemens shows, males treated with hormones showed decreased connectivity between the left frontoparietal cortex and the left dorsolateral prefrontal cortex. In other words, the hormone interventions decreased communication pathways in unintended ways in the brain. One might say that this has the effect of further deepening the body perception disorder, rather than working to resolve it. Not a desirable effect!
Impacts to Neural Networks and Astrocytes
Wrong sex hormones also damage astrocytes, the “glue cells” of the central nervous system, which are critical to brain function and stability. As Siracusa et al writes, astrocytes are …“a population of cells with distinctive morphological and functional characteristics that differ within specific areas of the brain. Postnatally, astrocyte progenitors migrate to reach their brain area and related properties. They have a regulatory role of brain functions that are implicated in neurogenesis and synaptogenesis, controlling blood–brain barrier permeability and maintaining extracellular homeostasis. Mature astrocytes also express some genes enriched in cell progenitors, suggesting they can retain proliferative potential.”
Simply stated, astrocytes have different properties and roles in brain function depending on where they wind up in the brain. Disorders of these cells, with a variety of brain function and blood-brain barrier and homeostasis-maintaining roles have been linked to a wide range of different neuro pathologies and mental disorders, such as schizophrenia, depression, and mood disorders (Koyama et al, Tarasov et al).
Wrong sex hormones create changes in these astrocytes, which are so critical to brain function. Currently, at the University of Madrid, researchers are using animal models to build a better understanding of the male and female brains subjected to wrong sex hormones. Their recent pioneering work on brain differences at the metabolite level, using magnetic resonance spectroscopy (1H-MRS), have come to several path breaking conclusions about brain morphology changes induced by the exogenous wrong sex hormone Estrogen and Estrogen with Cyprotone Acetate (CA- Anti-Androgen). They found that that exogenous estrogen, alone and with CA, leaches water from astrocytes, harming those cells in the process and causing several downstream effects, including brain volume loss.
In their concluding remarks, Gomez et al indicate that “Brain cortical volume correlated negatively with increased fractional anisotropy values and relative metabolite concentrations. These reveal a reduction in water content in brain cells, mainly in astrocytes but also in neurons and the oligodendrocytes surrounding their axons, as revealed by the increase of fractional anisotropy. Indeed, decreased cortical volume could be associated with neuro-cellular shrinkage, a circumstance that would disrupt the delicate metabolic equilibria among metabolite concentrations within neural cells”.
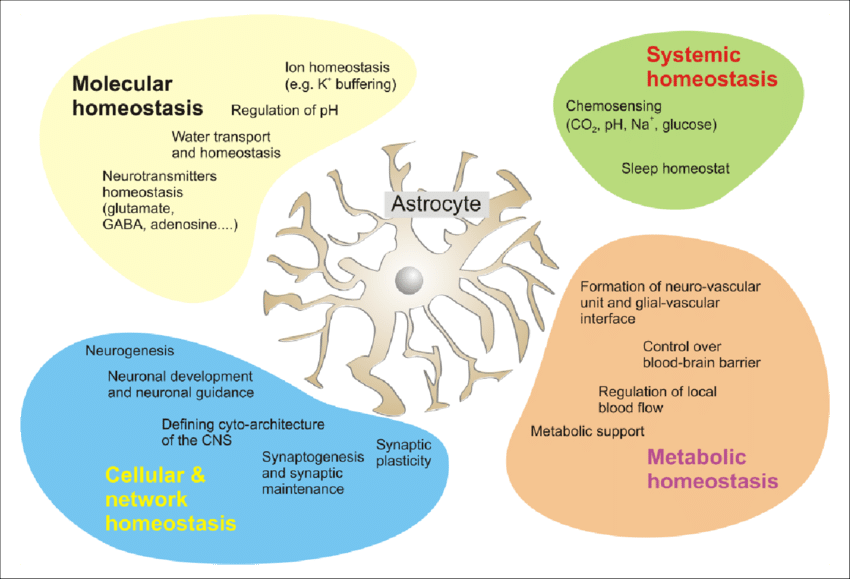
So, wrong sex hormones damage the cellular structure of astrocytes, which are critical to maintaining brain stability and function. And we know that disordered astrocytes are linked to various neuro-pathologies. We also know that wrong sex hormones reduce brain volume, likely due to the disruption of the delicate brain equilibrium. And, further, they decrease connectivity between areas of the brain, likely causing other issues yet to be discovered. Estrogenic shock to a still-developing male brain may explain continued psychopathology and mental health distress in wrong sex hormonally treated youth. It is likely that younger, still developing brains will not have the same resilience to astrocyte toxicity as might the much older males who have historically been the primary customers for wrong sex hormone treatments.
Progesterone is No Defense
Now that the risks of estrogen have been publicly raised for women and for men (transwomen), the common response from activists and gender doctors has been, don’t worry, we use progesterone in combination with estrogen — that is a protective hormone that makes estrogen totally harmless and safe! Progesterone is billed as a panacea in gender medicine for males (transwomen).
There are several issues with this argument. First, the information available is largely inapplicable to a male cohort. It does not hold that because studies have shown that it helps to protect the brain from estrogen in women (at levels used for post-menopausal women) — and so, therefore, it must do the same thing for men taking estrogen as a wrong sex intervention.
Progesterone use in Hormone Replacement Therapy (HRT) has been studied in women in several randomized control trials over the decades, such as the WHI, KEEPs and others. Specifically, these trials were conducting brain morphological studies, and determining if HRT was correlated with an elevated risk of breast cancer.
A study was conducted to determine the impact of hormone therapy on healthy post-menopausal women, using estrogen in combination with micronized progesterone (touted as the best option in a systematic review of progesterone use in women for HRT). This study of 77 women found that, after a 2-month trial, HRT led to an elevated risk of tumor gene expression. Yes, the results were better for micronized progesterone (an altered gene expression profile of 600 genes within the transdermal Estradiol and oral micronized progesterone arm, versus 2500 genes with equine estrogen medroxyprogesterone). And, of the 225 genes involved in mammary tumor development, 198 were attributable to medroxyprogesterone versus 34 for micronized progesterone. But, are better bad results acceptable? Both had adverse expression of important genes regulating proliferation, apoptosis and tumor inclination in vivo.
For postmenopausal women, there are also health benefits that help to counteract the risks of hormone therapy. In trans-medicine, we are talking about hormone therapy to develop superficial cosmetic features, like breasts (or more factually, gynecomastia in men and boys). There is no health benefit to males, apart from nebulous and disproven claims of improvements to mental health and decreased risk of suicide. In this case, how many tumor gene expressions are an acceptable risk to take after just 2 months of exogenous hormones?
In response to criticism about the inapplicability of studies on women to male cohorts, rather than admitting that conclusions should not be drawn for this reason, instead the researcher, Prior, challenges the critics to show evidence that the addition of progesterone is actually harmful! In other words, her expectation is to ask others to prove to her the converse of their argument, rather than expecting her to actually prove her claims.
Now, activists take these results from studies on women and restate them, ignoring the elevated risks of cancer, to conclude that men can expect full protection from the harmful impacts of exogenous estrogen by using progesterone. One can only assume that this is because they know that no one will bother to read the source materials. Even if we accept that progesterone mitigates any damage from exogenous estrogen, the data’s relevance cannot be extrapolated to draw conclusions about progesterone in males. Firstly, it is irrelevant because they are males with entirely different biology. And, secondly, it is inapplicable because estrogen is given to transwomen at 6 times the level used for hormone therapy in women!
There have also been studies on males undergoing wrong sex hormone therapy, and the results have also been terrible. Iwamoto, Safer et al cited a significantly enhanced breast cancer risk, in addition to increased risk of clots and stroke, with progesterone used concurrently. A total population study conducted in males, including transwomen, in the Netherlands found that, “There was a 46-fold higher incidence of breast cancer in the cohort than in cisgender men (standardised incidence ratio 46.7, 95% confidence interval 27.2 to 75.4). Most tumours were of ductal origin and estrogen and progesterone receptor positive, and 8.3% were human epidermal growth factor 2 (HER2) positive. A striking finding was that in trans women the risk of breast cancer increased in a relatively short time”. This is clearly not a desirable result.
Progesterone also does not improve mental health outcomes, as seen in the large cohort total population study reported by Pachankis et al, where progesterone was also used as a wrong sex hormone treatment and there was no resultant benefit to mental health.
Currently, progesterone in trans medicine (for transwomen) is being analyzed in WPATH SOC 8 with a “systematic review” but unfortunately, as usual, this is being done without the rigor of an actual double blinded randomized control trial, as noted by Iwamoto in a Letter to the Editor. Given the state of exogenous hormone replacement therapy even in women, any attempt to use progesterone in an adjuvant fashion as wrong sex hormones seems very premature, notwithstanding any “systematic” review by WPATH.
False conclusions, irrelevant cohorts, ignored studies—there is ample evidence that wrong sex hormone therapy is harmful and that progesterone doesn’t make it all better. So, why are doctors trying to demonstrate the safety and efficacy of progesterone? Because, as Prior notes, patients are demanding it. We cannot but be astonished about the lack of rigor in such public physician discussions about introducing a new and powerful exogenous hormone into the treatment protocol for males because patients are demanding it. And, they are demanding it, in a feat of circular logic, because certain so-called trans-medicine experts are touting it as a panacea. And around we go.
Five decades after the initiation of off label experimental hormone use for gender “transition’ on humans, we have yet to see the results of any randomized control trials, or FDA approved products. This is outrageous.

0.1mg Estradiol Transdermal Patch , FDA Warning
Above is the black box warning, required by the FDA for all products that have safety risks. This is what women prescribed estradiol patches receive, as that is the “on label” use of the drug. However, this disclosure never appears in “informed consent” for wrong sex hormones. In stark contrast, gender patients get puff pieces from gender clinics that downplay the risks and focus on slick marketing promising (or implying) rosy outcomes, full of fulfillment and happiness, in your new body.
In truth, we have no idea what the risks of these hormones are when used in trans medicine. The few studies into the risks and impacts of wrong-sex hormones in males point to very poor outcomes. Progesterone doesn’t make them safe. There is ample evidence that, as individuals ruminate on gender, they strengthen certain neuro networks, while others weaken. It is further known that behavioral substitution effects, instituted by reflection, detection, and conscious substitution, assisted by therapy or nootropics, can cause changes to these networks in more precise ways than can hormones. Instead of the nuanced impacts you can affect through traditional therapy, hormones instead cause broad astrocyte loss and long-term negative effects, not just on the DMN networks, but on the entire brain.
When damage to the brain, including leaching water from astrocytes, disruption to neural pathways and brain communication, reduction in brain volume, and high risk of cancers and neural-pathologies are expected outcomes, we should be hitting the “pause button” on medical transition and wrong-sex hormones, not hitting the “pause button” on children’s natural puberty and maturation process.
It’s abundantly clear that gender doctors have no idea what they are doing when it comes to medical “transition”. With astounding arrogance and an almost religious fervor, they are blindly meddling with the complex, nuanced instrument that is the human brain.
Nowhere does a brain test show up in any of the WPATH or USPATH SOCs, no cognition test, no mood or irritability tests, no serum BDNF levels or 1H- MRS studies in order to understand metabolite concentration changes over the duration of the wrong sex hormone treatment.
Short term euphoria is reported as evidence current treatments are safe and successful, long term impacts are not even measured. As, Gomez at al noted, with regret, with males on wrong sex hormones, the clinical follow up does not include systematic checking of brain structure and function. This is unacceptable. The only plausible reason for this willful ignorance is that gender doctors assume their treatments are dangerous, unethical and ineffective and are keen to avoid the liability that uncovering the truth will inevitably bring.
Gender medicine is governed by ideologues, not scientists. As a result, parents are in the absurd situation of having to prove why introducing wrong sex hormones into our children’s bodies (an absolutely insane idea) is a bad thing to do, rather than doctors and scientists proving to us that this “gender” medical intervention euphemistically called “transition” is safe and effective in helping our confused children with their societally-induced gender dysphoria.
This is an unconscionable disaster, a scandal of epic proportions, and no credible medical professional should proceed down this path. It’s time for immediate and drastic change. Enough. Doctors and researchers—start doing your jobs.
Sources
Bränström R, Pachankis JE. Reduction in Mental Health Treatment Utilization Among Transgender Individuals After Gender-Affirming Surgeries: A Total Population Study. Am J Psychiatry. 2020 Aug 1;177(8):727-734. doi: 10.1176/appi.ajp.2019.19010080. Epub 2019 Oct 4. Erratum in: Am J Psychiatry. 2020 Aug 1;177(8):734. PMID: 31581798. https://pubmed.ncbi.nlm.nih.gov/31581798/
Clemens, Benjamin et al. “Male-to-female gender dysphoria: Gender-specific differences in resting-state networks.” Brain and behavior vol. 7,5 e00691. 5 Apr. 2017, doi:10.1002/brb3.691 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5434195/
Collet S, Bhaduri S, Kiyar M, T’Sjoen G, Mueller S, Guillamon A. Characterization of the 1H-MRS Metabolite Spectra in Transgender Men with Gender Dysphoria and Cisgender People. J Clin Med. 2021;10(12):2623. Published 2021 Jun 14. doi:10.3390/jcm10122623 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8232168/
de Blok C J M, Wiepjes C M, Nota N M, van Engelen K, Adank M A, Dreijerink K M A et al. Breast cancer risk in transgender people receiving hormone treatment: nationwide cohort study in the Netherlands BMJ 2019; 365 :l1652 doi:10.1136/bmj.l1652 https://www.bmj.com/content/365/bmj.l1652
Gaudio, Santino et al. “Altered thalamo–cortical and occipital–parietal– temporal–frontal white matter connections in patients with anorexia and bulimia nervosa: a systematic review of diffusion tensor imaging studies.” Journal of psychiatry & neuroscience : JPN vol. 44,5 (2019): 324-339. doi:10.1503/jpn.180121 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6710091/
Gómez Á, Cerdán S, Pérez-Laso C, Ortega E, Pásaro E, Fernández R, Gómez-Gil E, Mora M, Marcos A, Del Cerro MCR, Guillamon A. Effects of adult male rat feminization treatments on brain morphology and metabolomic profile. Horm Behav. 2020 Sep;125:104839. doi: 10.1016/j.yhbeh.2020.104839. Epub 2020 Aug 22. PMID: 32800765. https://pubmed.ncbi.nlm.nih.gov/32800765/
Feusner, Jamie D et al. “Intrinsic network connectivity and own body perception in gender dysphoria.” Brain imaging and behavior vol. 11,4 (2017): 964-976. doi:10.1007/s11682-016-9578-6 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5354991/
Iwamoto SJ, T’Sjoen G, Safer JD, Davidge-Pitts CJ, Wierman ME, Glodowski MB, Rothman MS. Letter to the Editor: “Progesterone Is Important for Transgender Women’s Therapy-Applying Evidence for the Benefits of Progesterone in Ciswomen”. J Clin Endocrinol Metab. 2019 Aug 1;104(8):3127-3128. doi: 10.1210/jc.2019-00249. PMID: 30860591. https://pubmed.ncbi.nlm.nih.gov/30860591/
Kantarci K, Tosakulwong N, Lesnick TG, Zuk SM, Lowe VJ, Fields JA, Gunter JL, Senjem ML, Settell ML, Gleason CE, Shuster LT, Bailey KR, Dowling NM, Asthana S, Jack CR Jr, Rocca WA, Miller VM. Brain structure and cognition 3 years after the end of an early menopausal hormone therapy trial. Neurology. 2018 Apr 17;90(16):e1404-e1412. doi: 10.1212/WNL.0000000000005325. Epub 2018 Mar 21. PMID: 29661902; PMCID: PMC5902783. https://pubmed.ncbi.nlm.nih.gov/29661902/
Koyama Y. Functional alterations of astrocytes in mental disorders: pharmacological significance as a drug target. Front Cell Neurosci. 2015 Jul 6;9:261. doi: 10.3389/fncel.2015.00261. PMID: 26217185; PMCID: PMC4491615. https://pubmed.ncbi.nlm.nih.gov/26217185/
Manzouri A, Savic I, Possible Neurobiological Underpinnings of Homosexuality and Gender Dysphoria, Cerebral Cortex, Volume 29, Issue 5, May 2019, Pages 2084–2101, https://doi.org/10.1093/cercor/bhy090
McFadden, Kristina L et al. “Reduced salience and default mode network activity in women with anorexia nervosa.” Journal of psychiatry & neuroscience : JPN vol. 39,3 (2014): 178-88. doi:10.1503/jpn.130046 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3997603/
Moody TD, Feusner JD, Reggente N, Vanhoecke J, Holmberg M, Manzouri A, Sorouri Khorashad B, Savic I. Predicting outcomes of cross-sex hormone therapy in transgender individuals with gender incongruence based on pre-therapy resting-state brain connectivity. Neuroimage Clin. 2021;29:102517. doi: 10.1016/j.nicl.2020.102517. Epub 2020 Dec 2. PMID: 33340976; PMCID: PMC7750413. https://pubmed.ncbi.nlm.nih.gov/33340976/
Murkes D, Lalitkumar PG, Leifland K, Lundström E, Söderqvist G. Percutaneous estradiol/oral micronized progesterone has less-adverse effects and different gene regulations than oral conjugated equine estrogens/medroxyprogesterone acetate in the breasts of healthy women in vivo. Gynecol Endocrinol. 2012 Oct;28 Suppl 2:12-5. doi: 10.3109/09513590.2012.706670. Epub 2012 Jul 27. PMID: 22834417. https://pubmed.ncbi.nlm.nih.gov/22834417/
Prior JC. Progesterone Is Important for Transgender Women’s Therapy-Applying Evidence for the Benefits of Progesterone in Ciswomen. J Clin Endocrinol Metab. 2019 Apr 1;104(4):1181-1186. doi: 10.1210/jc.2018-01777. PMID: 30608551. https://pubmed.ncbi.nlm.nih.gov/30608551/
Ramírez-Barrantes, Ricardo et al. “Default Mode Network, Meditation, and Age-Associated Brain Changes: What Can We Learn from the Impact of Mental Training on Well-Being as a Psychotherapeutic Approach?.” Neural plasticity vol. 2019 7067592. 2 Apr. 2019, doi:10.1155/2019/7067592 https://academic.oup.com/cercor/article/21/11/2525/275208
Ratnakumar A, Zimmerman SE, Jordan BA, Mar JC. Estrogen activates Alzheimer’s disease genes. Alzheimers Dement (N Y). 2019 Dec 9;5:906-917. doi: 10.1016/j.trci.2019.09.004. PMID: 31890855; PMCID: PMC6926344. https://pubmed.ncbi.nlm.nih.gov/31890855/
Savic Ivanka, Arver, Stefan. Sex Dimorphism of the Brain in Male-to-Female Transsexuals. Cerebral Cortex, Volume 21, Issue 11. November 2011; 2525–2533. https://doi.org/10.1093/cercor/bhr032
Siracusa R, Fusco R, Cuzzocrea S. Astrocytes: Role and Functions in Brain Pathologies. Front Pharmacol. 2019 Sep 27;10:1114. doi: 10.3389/fphar.2019.01114. PMID: 31611796; PMCID: PMC6777416. https://pubmed.ncbi.nlm.nih.gov/31611796/
Stute P, Wildt L, Neulen J. The impact of micronized progesterone on breast cancer risk: a systematic review. Climacteric. 2018 Apr;21(2):111-122. doi: 10.1080/13697137.2017.1421925. Epub 2018 Jan 31. PMID: 29384406. https://pubmed.ncbi.nlm.nih.gov/29384406/
Tarasov VV, Svistunov AA, Chubarev VN, Sologova SS, Mukhortova P, Levushkin D, Somasundaram SG, Kirkland CE, Bachurin SO, Aliev G. Alterations of Astrocytes in the Context of Schizophrenic Dementia. Front Pharmacol. 2020 Feb 7;10:1612. doi: 10.3389/fphar.2019.01612. PMID: 32116664; PMCID: PMC7020441. https://pubmed.ncbi.nlm.nih.gov/32116664/
Verkhratsky A, Rodríguez JJ, Steardo L. Astrogliopathology: a central element of neuropsychiatric diseases? Neuroscientist. 2014 Dec;20(6):576-88. doi: 10.1177/1073858413510208. Epub 2013 Dec 3. PMID: 24301046. https://pubmed.ncbi.nlm.nih.gov/24301046/
Originally published at https://pitt.substack.com/p/transgender-medical-interventions reproduced by kind permission.